2023 Brian's Neck Surgery
(9/11/2023)
![]()
2023 Brian's Neck Surgery(9/11/2023)
|
 |
Timeline:
- 5/20/2019 Monday - in California - Brian has sudden pain
in left shoulder blade and neck - hurts to cough
- 5/26/2019 Sunday -
Brian goes to Urgent Care - Dr Wang says it is pinched nerve in shoulder,
prescribes anti-inflammatory
Prednisone
- 5/29/2019 Wednesday - Brian sees Primary
Care - Dr Roey disagrees and thinks neck injury, orders MRI to confirm,
prescribes Gabapentin
(nerve pain killer)
-
6/4/2019 Tuesday - Brian gets MRI (earliest possible appointment)
-
6/6/2019 Thursday - Doctors first look at MRI, Dr Roey calls Brian and says it
is bad, Brian sees new Physical Medicine specialist Dr Perkash in person who
says "needs surgery"
- 6/7/2019 Friday - Brian sees surgeon Dr
Wachhorst who says "not ER critical/dangerous, but requires surgery soon"
so schedules for
6/20/2019 which is first opening
- Pandemic - while researching
various options like total disc replacement, the pandemic hit and the hospitals
told me "go away, you can wait"
- 7/1/2023 - got a recommendation from
Lindsey Whalen
(anesthesiologist) for Dr. Michael Moghimi as a spine surgeon in Austin.
Saw Dr Moghimi around this time.
- 7/11/2023 - drove to Dallas to see
Dr Jack Zigler and
get another opinion.
- 8/17/2023 - last visit with Dr Moghimi (surgeon)
in Austin before I see him on the
day of the surgery (see two lines down)
- 8/25/2023 - PM&R (nerve conduction test, Electromyography) -
https://en.wikipedia.org/wiki/Nerve_conduction_study - carpal tunnel on
right arm/wrist
- 9/11/2023 - Brian undergoes "Anterior
cervical discectomy and fusion (ACDF)" performed by surgeon Dr Michael
Moghimi at
http://www.austinspinemd.com/
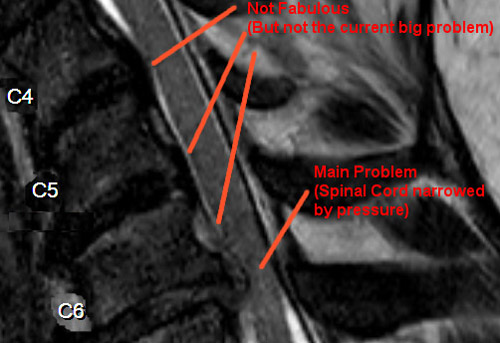
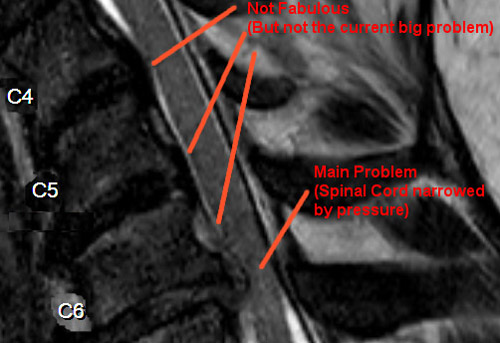
MRI Screenshot of THE PROBLEM:
Diagnosis: "Cervical Stenosis"
Herniated Cervical Disk c6/c7, Cervical Radiculopathy
I added the red text on the MRI screenshot below to help describe that my main issue is a bulged disk between vertebrae C6 and C7 causing pressure on my spine. In the picture below, the doctors said the white spinal fluid sack SHOULD be the thickness it is between C2 and C3, and that the reduction in spinal fluid sack thickness from C3 - C6 "is not good, but not the cause of my immediate pain and possible danger". The biggest problem is the meniscus (disk between vertebrae) between C6 and C7 is pushing on my spinal cord, causing pain. The reason I feel it in my left shoulder also is because that is exactly where the nerve travelling to my shoulder connects.
Neck Brace:
Brian will wear a neck brace 24/7 (including while sleeping) for the first week
after surgery.
The NIH says
this is useless and based on obsolete and incomplete information. Dr
Moghimi says it is for my comfort and I can take it off when I like.
Pictures from Just After Surgery:
Below is a panorama of my private room at Northwest Hills Surgical Hospital, located at 6818 Austin Center Boulevard, Austin, TX. In this particular facility, they always have 1 staff member for every 3 patients, and there are only 9 beds total. I was very happy with their care. I've had some horrible hospital experiences so I am always worried about it, but they really did do everything well here.
In the picture below I highlighted in red the "Bair Paws" device. It blows warm air down a tube, kind of like a blow dryer on "low". My gown had "ports" that you can plug the "Bair Paws" into. Or the patient can put the disconnected end under their blanket to stay warmer. I've never seen anything like this before.
A close up of the "Bair Paws" system.
A panorama of my private bathroom.
After I woke up from general anesthesia, I had not eaten in about 20 hours. The nurses/staff gave me some choices of food and this was my first meal.
Okay, so the "Voldyne 4000" seen below is this odd device called an "incentive spirometer". You can get it for $8 at Walmart. You blow in the tube trying to keep the little green disk over the "happy face" seen at the center of the picture below. Supposedly this helps avoid pneumonia by exercising the lungs and inflating the lungs. I sleep with a CPAP (even in this hospital) and I'd make the bold claim the CPAP is better at inflating my lungs, but whatever...
A picture I took in the bathroom mirror to show what is going on at this point. I woke up from surgery wearing the neck brace I'm wearing in the picture. I have a drain tube embedded about 8 inches into my neck draining into the "body fluid hand grenade" hanging on my chest and it filled with fluid every 10 hours or so and the nurses would empty it somehow. Finally, see the big "belt" I'm wearing? When I'm in bed or sitting in a chair the nurses take that off of me. But they REALLY didn't want me standing up by myself without a nurse or assistant present RIGHT THERE beside me, and they scolded me several times when they discovered I was out of bed wandering around alone (like taking the selfie seen below). They would put that belt on me and then hang onto it with one hand as a "handle" supposedly in case I started to fall. But most of the nurses were about 5 feet tall and 100 pounds soaking wet, and I am 6 foot 3 inches tall and weight 280 pounds. I should be lifting the nurses with a handle, not the other way around.
Below is a close up of the surgery incision. It's impressive they could make such a small incision and insert all sorts of titanium hardware through the incision, then drill my bones and screw titanium screws into plates and bone. All through this small hole in my throat.
Below is a movie of a few hospital experiences. It is 5 minutes long and kind of random cut together little experiences. But it does show the drain being pulled out of Brian's neck! Click here for the highest resolution original version.
I barely got any sleep the first night. My surgery was over by 4pm and I was in my private room. They were very consistent at coming in every 4 hours and giving me pain medications. But between the discomfort from surgery and the fact that the bed didn't recline I really didn't sleep much. The next morning they offered me a few different things for breakfast and I had the breakfast sandwich seen below. It was actually quite good! I was shocked they offered coffee, and they said "it isn't very good coffee", LOL. But I thought it was fine. About breakfast time and with a little coffee I finally was feeling more "normal" after the general anesthesia effects finally wore off.
Oh, side story: I'm old and have been hospitalized several times before, and I alerted them I was going home this day (the day after surgery after 1 night in the hospital). Now, they try to talk you out of this, but there are several good reasons to leave the hospital, not the least of which is each day spent in the hospital is like the world's crappiest spa that costs THOUSANDS of dollars per day. They don't tell you this, but one of my previous stays was about $8,000 per day. Since insurance rejects a lot of claims nowadays, it's in your financial interest to go home as soon as possible. If anybody says "no, you are staying" the correct term to use is "I'm leaving Against Medical Advice". AMA - Against Medical Advice. That's when they start moving faster and get you checked out. They don't have any ability to keep you there legally. I usually give them a deadline several hours in the future, like if the breakfast below was at 6:30am I say, "I'm leaving AMA at noon. If you have all the paperwork done by then great, otherwise I'm walking out without doing the paperwork." These were REALLY sweet and nice and caring people (I was impressed by how "nice" this hospital experience was compared to pretty much all my previous hospital stays), and I was polite and explained they didn't do anything wrong, I just wanted to go home to recover.
There is a whiteboard like this in each of the patient's rooms. They only have 9 "beds" in this facility, and always at least 3 staff there to take care of the patients. When they did things like give me pain meds, they quickly updated the whiteboard. It also had the names of all the staff that was there with me, so they came in and changed it all at "shift change". Randomly, the nurses here worked 12 hour shifts, 3 days a week. So only 36 hours/week of work. I have no idea why it makes sense to them to have 12 hour shifts, but whatever, I don't care. It is not my monkey, not my circus.
The picture below is a close up of what the "patient whiteboard" contains. One of the things I learned is unless you say your pain is a "4" or above and use the correct emoji as your facial expression, you don't get the pain medications. It's really helpful that they show you how to hold your face with the emoji!! I was saying my pain was a "1" so I could leave the hospital without a hassle. My pain was actually more like an "8", but you can't ever be honest with them about this, you start with your goals (leave hospital) and work backwards into what number you tell them for the "Pain Scale". I kept telling them my pain was a "1" and using the happy emoji expression so I could leave, meanwhile it was getting harder and harder to cover up the excruciating pain. Then right before I signed the discharge papers I said, "hey, my pain is really temporarily a 4, can I get one more pain pill?" That seemed to work for them and they gave me an overdue dose of pain meds. Then I told them my pain returned to a "1" after I swallowed the pill and I checked out and left the hospital.
BEFORE surgery when I was hanging out waiting in the "pre-operation" area, they put in the "implanted medical port" in my vein seen below. It stays in through the surgery and stays in as long as you are in the hospital (so potentially for days). They had to take this "port" out before I left the hospital, but I could have done it myself if they weren't willing to. This port is a really good idea. Since my vein is already "tapped" with the port installed, if there is an emergency and they need to give me injection meds, it is super easy and fast. They also used the port to give me some sort of healing steroid once, maybe twice while I was there. They "flushed" the port with saline from time to time. Once in the morning just as preventative measure, then before they gave me the healing steroids.
In the picture below you can see they also gave me a concert style wrist band. I'm not sure why they gave me a concert wrist band? I mean, I couldn't find any live music in the hospital, but since this is Austin I wouldn't be surprised if they had live musical acts sometimes.
Immediately after I woke up from surgery, they put the two wrist bands on my other hand. One of them used the acronym: "NKDA" which means "No Known Drugs Allergies". I think this makes sense like as nurses hand off responsibilities at the end of their shift it's good that a very simple system is attached to me listing my drug allergies.
The OTHER wrist band is bogus. It isn't actionable. It just says I'm clumsy and might fall down. I felt like a puppy wearing a cone of shame with that one. Even when I was doing nothing wrong, I was marked.
A picture of what is behind me when I'm in the bed.
Finally home on 9/12/2023 at about 1:30pm! In the picture below that I'm taking in a mirror you see the neck brace and the incision.
Picture below without the neck brace.
Close up of the incision.
On 9/19/2023 - 7 days after surgery I took off the bandage, and this is what the incision looks like (see picture below). Remember, you can click on any image for a zoomed in version. It really is impressive that they can do this much work through the small incision.
Two weeks post op X-ray side view:
Two weeks post op X-ray front view:
For completeness and out of order, the MRI on 6/27/2023 click here1_neck and here2_lower_back.
Alternatives that Brian did not have done::
-
there is a newer, better procedure called
Total
Disk Replacement (TDR) where a FLEXIBLE device is implanted instead of
fusing the spine solid (no flex).
The M6 is an example
of the device. Also
the ativL. Unfortunately Brian needed 3 discs removed/replaced, and
only 2 levels are recommended, so in the end Brian went with the older ACDF
procedure.
Imaging includeing MRI, CTscan, and 2 X-rays:
-
Click this Link for an MRI ZIP of the
most recent 2023 MRI
-
Click This Link to Download an MRI ZIP file of BrianW's
spine/Neck (about 100 MBytes, so super tiny by modern standards!)
- Click This Link to
Download a ZIP of a CTscan, and 2 X-Rays of Brian's Spine. (about 100
MBytes, so super tiny by modern standards!)
INSTRUCTIONS
ON A WINDOWS PC (Note: this is not my fault, it is Sutter Health Medical who
wrote this!!!!):
1) Download the file
2) Unzip file the file somewhere (I am VERY SERIOUS about this, it will not run
directly from the ZIP contents!!!!)
3) Double Click the file called "start.hta" and it will lauch a program that
allows you to view the MRI and other images
Hopeful Outcome?
- Hopefully Brian will be cured
forever, and only have about 10% - 15% reduction in neck mobility (which is fine
for a software engineer).
Research Notes
- Neck Braces don't help. The
National Institutes of Health (NIH) says: "Conclusion:
We recommend against the routine use of ECO after ACDF due to a lack of improved
fusion rates associated with external bracing after surgery."
- My
original (2019) surgeon proposed doing
ACDF and implanting: The interbody implant is
Titan Endoskeleton (TC or TL?). The plate and screws are
Synthes CSLP Cervical Spine Locking Plate.
- My 2023 (actual) surgeon Moghimi did ACDF and implanted: "GMA anterior
cervical system, 7-mm PEEK interbody cage x3 (3 of them), 63-mm anterior
cervical plate (1 of them), demineralized bone matrix (cadaver bone).
- An alternative surgery is called
Total
Disk Replacement (TDR) or
Artificial disc replacement (ADR) where an artificial disk is inserted which
allows motion after the surgery (instead of disk fusion). The FDA
products approved for neck are:
1)
Synthes Spine ProDisc-C
,
2)
Prestige LP by Medronics,
Medronics Website about it,
3)
Mobi-C Cervical Disc made by
LDR who is now
Biomet. "In
the two-level study Mobi-C demonstrated SUPERIORITY to ACDF..."
4)
M6-C or
M6-L?,
Spinal Kinetics Dynamically Stable Cervical Disk Replacement.
5) The activL by company
"Aesculap" may not be FDA approved yet, but Dr Richard Guyer likes it.
-
Dr. Michael Moghimi - Lindsey Whalen recommendation -
http://www.austinspinemd.com/
- Dr Robert Masson - Florida - recommended by Dr Volpe -
https://massonsi.com/ Masson Spine Institute
-
Dr Richard Guyer (worked on Tiger Woods) in Texas.
Google Reviews.
Article about 15 years of Total Disk Replacement by him.
-
Dr Todd Lanman (Los Angeles).
Press Release.
“Though the short
term results may be similar to fusion, the real difference comes with long term
follow up of greater than 5 years. The fusion patients are up to 3 times more
likely to have surgery at the next level compared to the disc replacement
patients.”
"I see my patients who have been lucky enough to be covered
(by their insurance) for artificial discs and those who were denied by their
insurance carrier and had to have fusion surgeries."
MRI Screenshot:
Diagnosis: "Cervical Stenosis"
Herniated Cervical Disk c6/c7, Cervical Radiculopathy
I added the red text on the MRI screenshot below to help describe that my main issue is a bulged disk between vertebrae C6 and C7 causing pressure on my spine. In the picture below, the doctors said the white spinal fluid sack SHOULD be the thickness it is between C2 and C3, and that the reduction in spinal fluid sack thickness from C3 - C6 "is not good, but not the cause of my immediate pain and possible danger". The biggest problem is the meniscus (disk between vertebrae) between C6 and C7 is pushing on my spinal cord, causing pain. The reason I feel it in my left shoulder also is because that is exactly where the nerve travelling to my shoulder connects.
Longer Version of Story for those interested::
On Monday, 5/20/2019 I woke up and my left shoulder and neck was in severe pain for no reason.
Sunday, 5/26/2019 - After a week of not getting better at all, I went to
Urgent care on Sunday, 5/26/2019 and
Dr Victoria Wang mis-diagnosed me as "Suprascapular
nerve entrapment" (pinched nerve in shoulder) and she prescribed 5 days of
Prednisone (as a strong anti-inflamatory). Dr Wang gave no other guesses or a
percentage chance she was correct, she just handed me the final diagnosis, and a
couple printed sheets describing this condition (which I do not have) and how it
might require as much as a cortisone injection and some physical therapy.
Wednesday 5/29/2019 - I followed up with an appointment with my primary care
doctor as soon as someone could see me, and my main doc was on vacation so I got
in to see Dr Steven Roey (stand in replacement) on Wednesday 5/29/2019. Dr Roey
immediately disagreed with the previous diagnosis and said "I think it is in
your neck, not your shoulder at all" and even said he thought it was a pinched
nerve in my neck in a particular location. He thought the Prednisone was useless
but I was only a dose away from completion so he said "finish it just so we can
say you tried that" and Dr Roey said "but we are all just guessing so let's find
out who is right with an MRI".
Tuesday, 6/4/2019 - The first time I could get an MRI was on Tuesday, 6/4/2019,
in the afternoon. This 7 day wait is because the hospital (Sutter Health in
Mountain View) own this $3 million piece of hardware that can diagnose things
deep in the human body without harming one cell, but they only run it a very
limited number of hours M - F, and NEVER on the weekend, and there is a long
line of people in pain who would like to pay them money to use it. They COULD
allow people in extra pain to bonus them more money (in addition to insurance)
and run it after hours, all night long, but they are REALLY BAD AT BUSINESS (and
arguably health care) so they just allow long wait times for people in pain and
who are dangerously mis-diagnosed (like me).
I found it particularly interesting that the waiting room for the MRI was filled
with people like me - twisted people hunched over wincing in pain some with
visible injuries. So I got the MRI. It took 15 minutes of lying on a flat slab
motionless wearing ear plugs. A shaved monkey could operate this completely
automated MRI machine - the machine did all the work automatically and spoke to
me in a clear woman's voice about what was going to occur next. Mostly the
machine made loud noises for either 30 second intervals or 4 minute intervals,
and rested for a minute or two between scans. Sometimes it moved my flat slab I
was lying on a few inches.
The whole thing took 15 minutes, as I left another person in pain was getting
loaded onto the flat slab of the MRI machine as fast as possible to keep this
pipeline going. Honestly, it could be done as a self serve thing with no
technician and a kiosk to sign into. Safeway self checkout is more complicated
than this.
Thursday, 6/6/2019 - Dr Roey had referred me to a Physical Medicine and
Rehabilitation doctor to interpret the MRI, and the first one that could see me
in network after the MRI was Dr Rajan Perkash on Thursday, 6/6/2019 so another 2
day delay.
Thursday, 6/6/2019 - 8am while driving - So on Thursday, 6/6/2019 as I was
driving to my 8:30 am appointment with Dr Perkash, Dr Roey called
my cell phone, and Dr Roey scared the crap out of me the way he was saying he
just saw my MRI for the first time and that I definitely needed surgery and it
was "very bad and needs immediate spinal surgery".
Thursday, 6/6/2019 - 8:30am Dr Appointment - So I was a little freaked out and getting used to this idea as I went to my appointment with Dr Perkash. Now, I want to point out I knew the diagnosis already, but to "check into a doctor" they did the standard incompetent "1920s medicine act" measured my weight and took my temperature and blood pressure to check me into this appointment. Like always, I had to fill out a piece of physical paper saying what my problem was. I had to write my own name at the top, because the technology to print out paper with my name hasn't been adopted by hospitals yet. You check into flights at the airport on a kiosk, you order meals at TGI Fridays with a wireless pad, but doctors can't seem to move out of 1953. So after these artificial delays, I met with Dr Perkash for the first time 30 minutes later, and Dr Perkash ALSO was extremely agitated and mentioned the "very bad MRI" and gave me a bunch of physical tests like "pull against my arm" and "do you feel this pinch equally on both arms of your body". Dr Perkash was VERY SURPRISED that I wasn't in worse condition and that very little permanent nerve damage had been done yet, given the horrible MRI results I had not seen yet. (Remember, this was the first time I ever met Dr Perkash.)
Thursday, 6/6/2019 - 9:00am - Dr Perkash then finally showed me the MRI for
the first time with the pinched spinal cord between C6 and C7 vertebrae. Dr
Perkash kept saying "there is only one solution and that is surgery". No
cortisone, no Chiropractor, no Chinese medicine, don't wait, get surgery NOW.
I should mention Dr Perkash is not a surgeon, more of a physical medicine
specialist for things like rehabilitation and physical therapy.
Friday, 6/7/2019 - 8am next day Surgeon consult - From this point onward there
were no more long waits for me for medical help or tests. I saw the surgeon the
VERY NEXT DAY because he simply cancelled on another patient to clear his
schedule to see me. This scared me even more, because it was so strange to see
doctors actually doing things quickly like seeing patients with less than a 6
week wait. The surgeon I saw is
Dr Scott
Wachhorst.
Dr Wachhorst gave me a ton more physical tests and was glad to see that I did
not have much nerve damage (or any nerve damage) because he had already seen my
MRI. Dr Wachhorst also went through my MRI and spent quite a bit of time showing
me different views and parts and explaining things much better. To
determine exactly which type of surgical procedure to do (mainly whether to
relieve the pressure
on one side of the spinal cord or the other), Dr Wachhorst wanted two more
X-Rays and a CT scan to figure out if a shadow on the MRI was "calcified".
If it was "calcified" the surgery would be to make space on the OTHER side of
the spinal cord by removing some bone over there and that surgery would NOT be
done by Dr Wachhorst. The X-Rays and CT scan showed no calcification so
the surgery would be done by Dr Wachhorst. To prepare for surgery Dr
Wachhorst also wanted an uptodate EKG, Urinalysis, and blood work to make sure
there is a good chance I could survive the 6 hour surgery under general
anethsesia.
Dr Wachhorst had a more calm diagnosis than the previous two doctors. He said this took years to get this bad, and my head isn't about to fall off, and that if it was that serious he would be sending me to the ER to do the surgery immediately, but it isn't that much of a panic. His first available surgery slot is 6/20/2019, and after that he is on vacation for a few weeks so why don't we take care of it. However, he did NOT like the idea of putting it off for two or three months, that made him uncomfortable.
Friday, 6/7/2019 - 9:30am - 11:30am - The X-Rays, CT Scan, EKG, Urinalysis, and blood work were all done IMMEDIATELY after I walked out of Dr Wachhorst's office in the same hospital. All of these things happened instantly with no wait, I just walked out of Dr Wachhorst's office and into each test department one after another and they did each test - no more multi-day waits. It was kind of what I might like medicine to be like normally, except it was kind of scary how each test technician said hello, pulled up my record on their computer, frowned, looked back at me for a second, then looked back down and started moving faster than normal and looking worried. That part was unsettling. I left the hospital after the last test and drove towards work.
Friday, 6/7/2019 - noon - as I arrived at work, I got a phone call from Dr
Wachhorst's assistant saying I needed to come pick up instructions for the day
of the surgery, plus a neck brace for the day of the surgery (I will wake up in
the neck brace), plus she wanted to give me some surgical sponges filled with
antibiotics that I use the night before surgery to clean my neck before I sleep,
then the morning of surgery to clean my neck, then they will still scrub my neck
when I get to the hospital. So I turned around and drove the 30 minutes
BACK to the hospital to pick all this stuff up and get all the explanations
about not eating or drinking after midnight.
Monday, 9/11/2023 - The Surgery Dr Moghini Performed
The procedure is called:
"Anterior cervical discectomy and fusion (ACDF)" which
is to enter through the front of my throat, stretch my
vocal cords out of the way (not cut them), stretch some
other tendon stuff out of the way (not cut them), move my esophagus out of the
way (not cut it), then
drill right down the center of the meniscus (the cushion
between the vertebrae) to reach the bulges and remove
them. Thus removing the pressure on my spinal cord.
This leaves a gap in the meniscus, so to repair that
they insert a titanium box with holes to allow bone to grow through it, and fills
the box and area around with chips of cadaver bone
and then the doctor
also puts in a plate or "strap" on the the spine
to stabilize it. Titanium is not affected by magnets,
so I can still get MRIs in the future after having this done. I
The procedure takes about 30 minutes per vertebrae.
Plus the time to open and to close. So it's
a big 2+ hours under general anesthesia.
So that's about it for now.
![]()